Minding gaps in revenue cycle technology to support value-based care
How organizations are adapting to CMS 2030 goals through innovations in revenue cycle management and strategic partnerships, measuring progress through a new framework.

Traditional fee-for-service reimbursement models, which focus on quantity rather than quality of care, are steadily being replaced by VBC models that align incentives with patient outcomes. The CMS 2030 mandate centers around driving accountable care in the following ways:
- • All Medicare fee-for-service beneficiaries will be in a care relationship with accountability for quality and total cost of care by 2030.
- • The vast majority of Medicaid beneficiaries will be in a care relationship with accountability for quality and total cost of care by 2030.
To achieve this CMS goal, healthcare provider organizations are modernizing their technology infrastructure in many areas. Upgrading revenue cycle management (RCM) technology to include AI and automation is a top priority for healthcare executives, according to a recent HFMA survey.
This article highlights the significance of advanced RCM technology to support value-based care and achieve the CMS 2030 goals in healthcare. It also introduces a new adoption model framework to benchmark your organization’s use of RCM technology and identify key RCM technology gaps.
Assessing revenue cycle technology readiness
While payment models will change under value-based care, healthy margins and financial sustainability remain essential for healthcare provider organizations to support their communities. Modernized RCM platforms hold the key to achieving these goals. But how do organizations know if their current systems are data-driven and ready for value-based care?
A vendor-agnostic adoption model provides a framework for revenue management that will help answer that question. Consider it a fresh take on the HIMSS Electronic Medical Record Adoption Model (EMRAM) that measures seven stages of clinical outcomes, patient engagement and clinician use of EHR technology.
This new revenue management version of EMRAM gives health system leaders a holistic view of their organization’s financial technology footprint, as well as key performance revenue indicators. It can be called the Revenue Management Technology Adoption Model, or RMTAM.
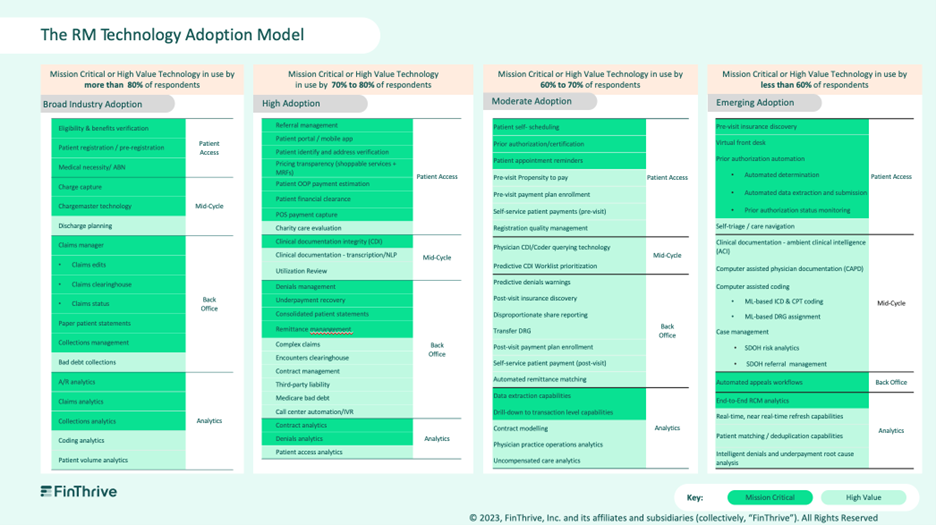
RMTAM was architected based on survey results and direct interviews with more than 100 health system revenue cycle leaders, resulting in detailed technology adoption assessments and financial performance reports from participants. More than 100 technology categories were studied as part of this research, spanning front, middle and back office point solutions, as well as analytics and automation.
Our research uncovered perspectives on which technologies were considered mission critical and must have by respondents vs. those that were seen as moderate or low value. The survey also quantified current market adoption of these capabilities among health systems.
This data was used to study the relationship between technology utilization and financial performance within U.S. health systems. The result of this research is the Revenue Management Technology Adoption Model, a five-stage framework that enables health system financial leaders to benchmark their organization against peers, and forecast impact to financial performance that could reasonably be expected as a result of modernization efforts.
Unpacking RMTAM
The Revenue Management Technology Adoption Model is a five-stage adoption model that is structured based on current industry adoption of technologies, where broadly adopted technologies are placed in Stage 1, and promising new technologies with low technology adoption are placed in Stage 5. RMTAM that aims to establish a starting point for the industry, what we are calling Stage 1, where a statistically significant portion of US health systems will find themselves.
More than 15 health systems are currently beta testing the RMTAM, providing ongoing feedback about their experience with the assessment itself and the strategic value a benchmarking framework like this has had for their organization.
Support for the initiative
There are three emerging benefits of conducting a revenue cycle technology assessment using the new adoption model. It can help organizations:
- • Gain insights to make well-informed decisions regarding the most suitable technology strategies and next steps.
- • Identify the current adoption stage and develop a revenue management roadmap that will achieve KPI-based revenue management goals under value-based models.
- • Navigate the evolving healthcare landscape as new value-based programs emerge with the ability to predict future financial performance.
As with all transitions, technology is only part of the equation. Culture, people and processes also must adjust for optimal revenue outcomes under value-based care. Now is the time for financial leadership to ready their teams, as well as technology, for the change.
Key strategies for value-based care
To propel the transition toward value-based care, health leaders play a pivotal role. Here are three leadership steps to consider in the year ahead.
Champion payment reform. This involves actively engaging with policymakers, payers and industry stakeholders to promote the adoption of payment models that incentivize quality outcomes and patient-centered care.
Equip providers with comprehensive education on VBC principles. Prepare healthcare providers through comprehensive education on the new model’s principles, strategies and best practices. Focus on topics such as care coordination, population health management, quality improvement methodologies, risk stratification and the use of data analytics for performance measurement.
Forge strategic partnerships with healthcare organizations and technology vendors. By working together, organizations pool resources, share expertise and leverage innovative technologies to drive improvements in care coordination, data exchange, analytics and patient engagement. These partnerships enable the development and implementation of integrated, patient-centered solutions that enhance the delivery of value-based care across the care continuum.
Jeff Becker is vice president of portfolio marketing at FinThrive.